They say that modern technology can be a good servant but a bad master - and it really is. From the point of view of a visually impaired user, a mobile phone, tablet and computer help me, among other things, at work, recognizing images and colors or navigating. In addition to having vision problems, I was diagnosed with type 2019 diabetes in July 1. Personally, I am of the opinion that a person should try to integrate into normal society as much as possible despite all health complications, but it was not easy at the very beginning of life with diabetes.
It could be interest you

Fortunately, I had, and still have, many people around me who were able to help me, including family, friends and sports coaches. Thanks to this, I can function with diabetes as well as I did before I was diagnosed. However, modern technologies that significantly facilitate the treatment of diabetes are an integral part of my everyday life. How did I get to them, what was a big but difficult nut to crack for me as a visually impaired person, and where did I get the most support?
What exactly is diabetes?
Many readers have probably met someone with diabetes before. However, not everyone knows what causes it and how it is treated. In very simple terms, it is a chronic disease in which the insulin-producing pancreas dies completely, i.e. if it is type 1 diabetes, or it is significantly weakened if it is type 2 diabetes. Type 1 diabetes cannot be cured in any way, it is a genetic defect that usually manifests itself after birth, during puberty or when there is a great deal of stress. Diabetes of the second type is acquired, and worse by lifestyle, excess of stressful activities or a passive lifestyle.

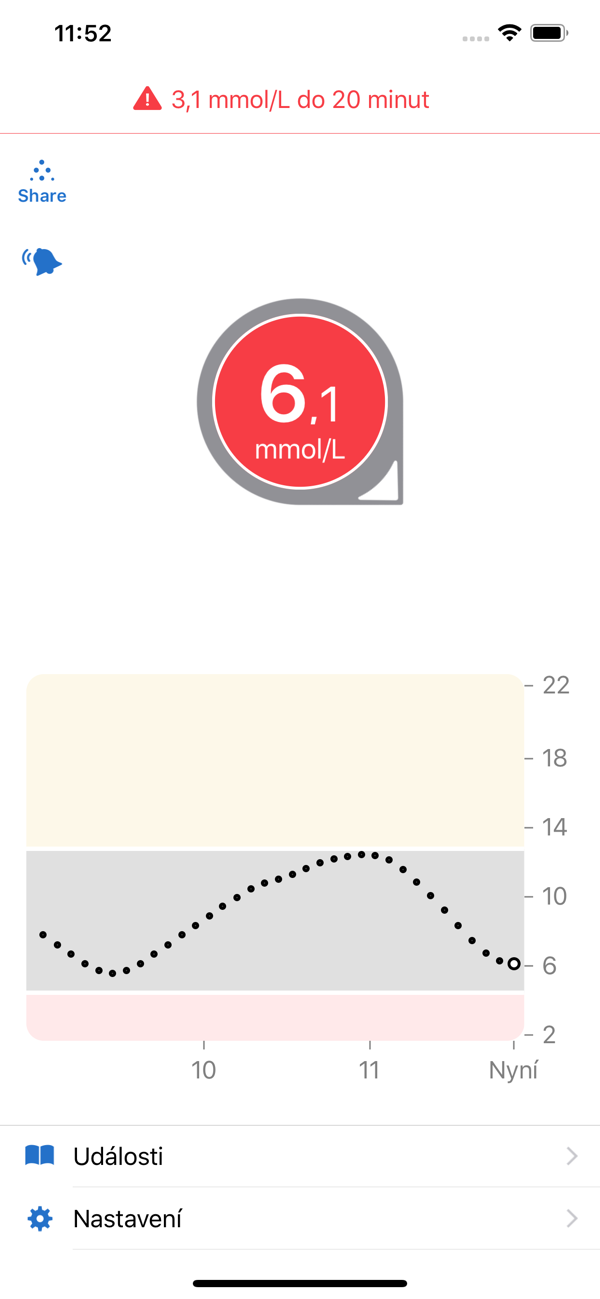
Insulin must be delivered externally, using insulin pens or a pump. If the patient has little insulin in the blood, the sugar in the blood rises. A condition in which a person has too much sugar in the blood is called hyperglycemia. Conversely, with a large amount of insulin in the body, the patient falls into hypoglycemia and it is necessary to consume carbohydrate foods to replenish sugar. Both hypoglycemia and hyperglycemia can in extreme cases lead to unconsciousness or death of the patient. Therefore, in order to keep the blood sugar level in the range, it is necessary to follow a regular diet and to supply insulin.
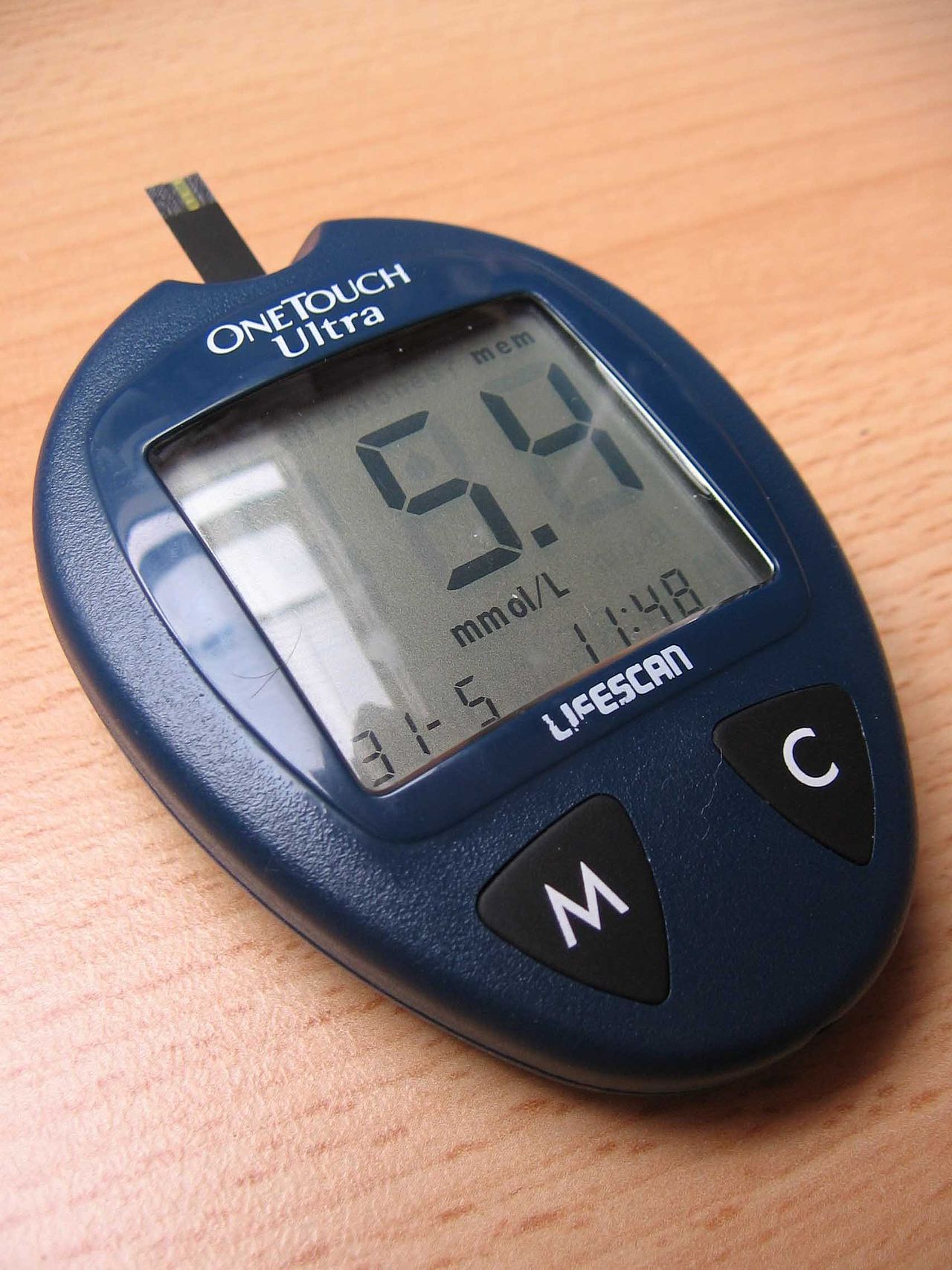
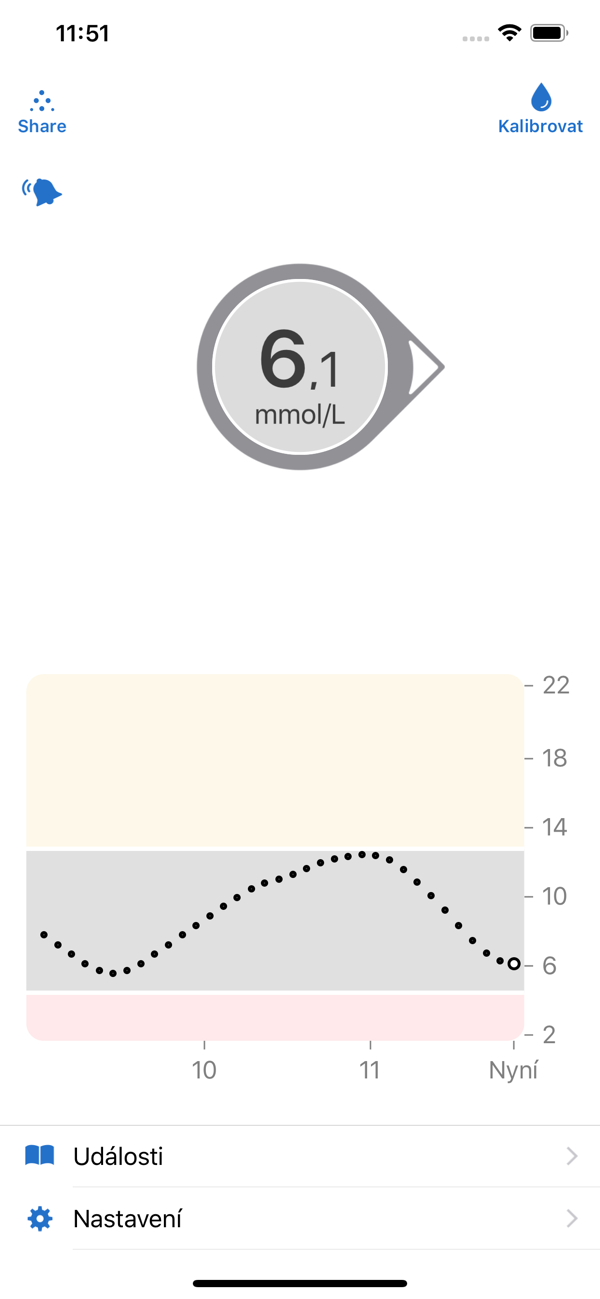
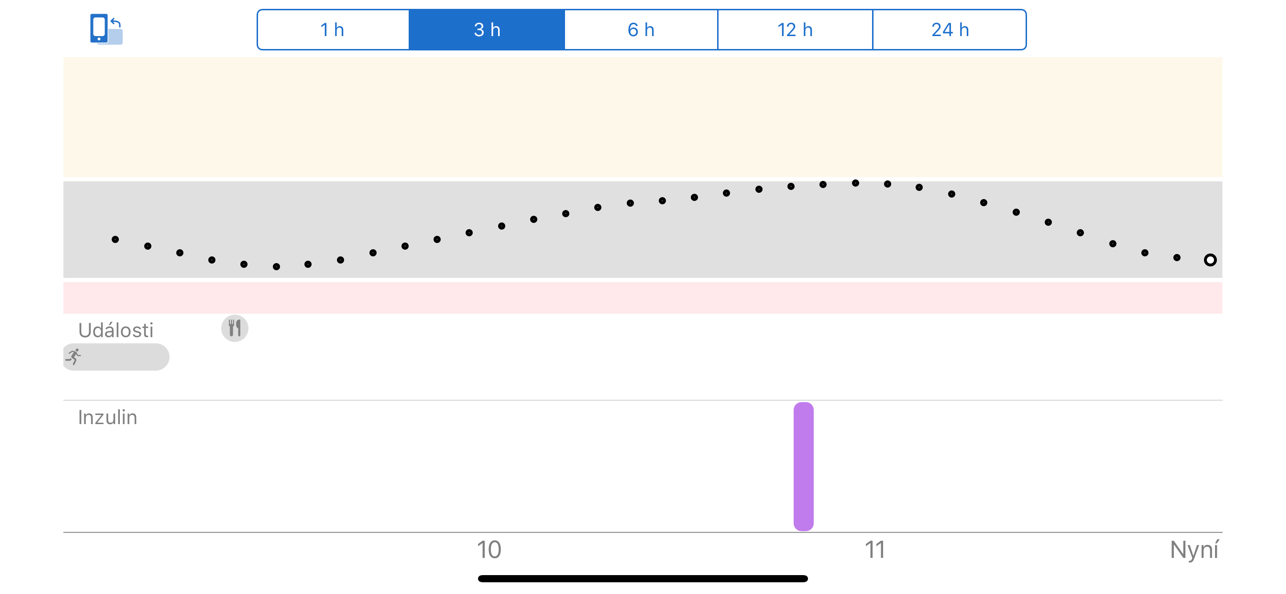
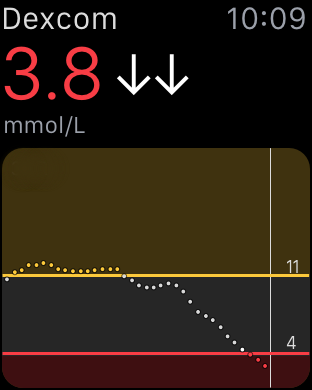
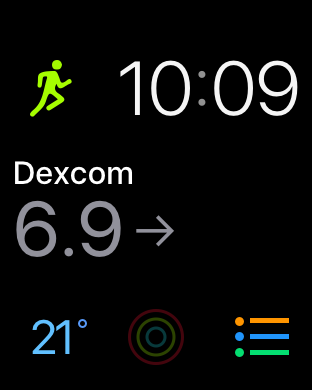
Blood glucose is measured using a glucometer or continuous monitor. A glucometer is a device on which the patient takes blood from the fingertip, and after a few seconds he learns the value. However, this measurement is not always completely comfortable, mainly due to its low discretion. In addition, after time, visible injuries start to appear on the fingers, which, for example, made it uncomfortable for me to play musical instruments. A continuous blood glucose monitor is a sensor that is constantly inserted under the skin of the patient and measures the sugar level every 5 minutes. The values are sent to the application in the mobile phone with which the sensor is connected via Bluetooth technology. I personally use the Dexcom G6 sensor, with which I am satisfied, both in terms of functionality and the accessibility of the program for the visually impaired.
You can try the Dexcom G6 app for iPhone here
Administering insulin is not that simple
As I have already outlined in the paragraphs above, insulin is administered either through an insulin pen or a pump. If you administer insulin with a pen, it is necessary to administer it 4-6 times a day with the help of a needle. Both the dosage and the injection itself can be handled with the help of a needle without any problems or blindly, but in this case it is necessary to place an increased emphasis on regular eating, which in my case, when I normally have a lot of sports activities or music concerts, was only hard to do.
It could be interest you

An insulin pump is an electronic device that is connected to a cannula in the patient's body. This must be replaced at least once every three days, so you need to inject much less often than when applying with insulin pens. In addition, the pump contains relatively advanced settings, where the patient can adjust the delivery according to food or physical activity, which is to a large extent more comfortable than the first mentioned method. I see the biggest disadvantage in the need to carry the pump with you all the time – during contact sports, it may happen that the patient pulls the cannula from his body and the insulin is not delivered to him.

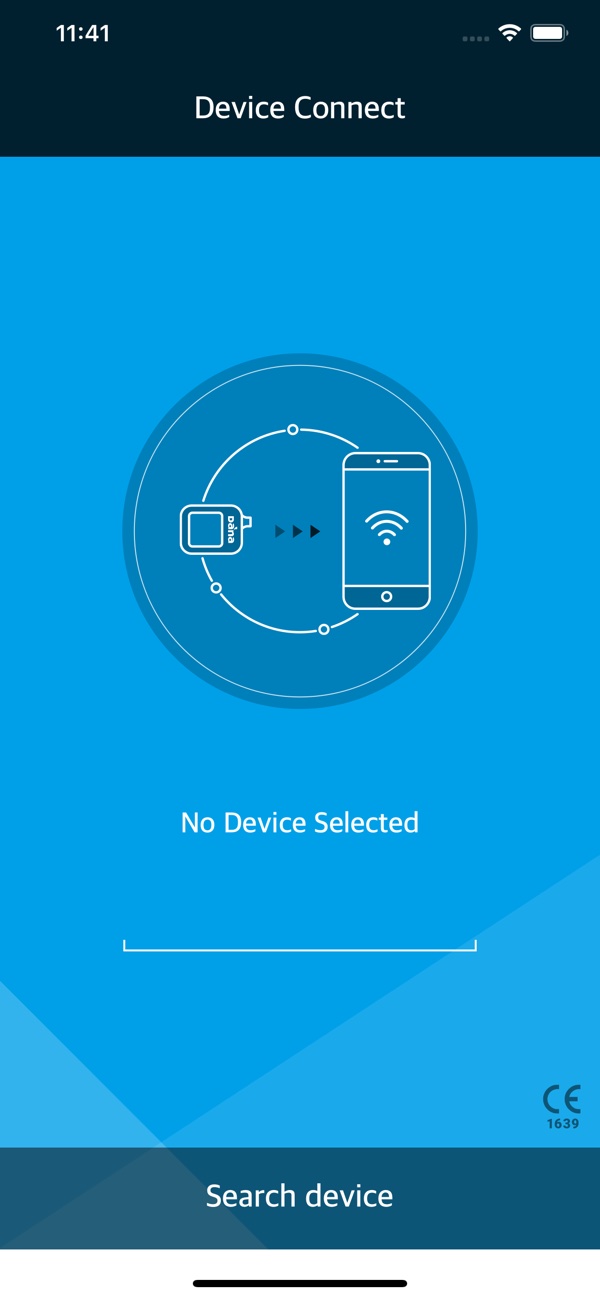
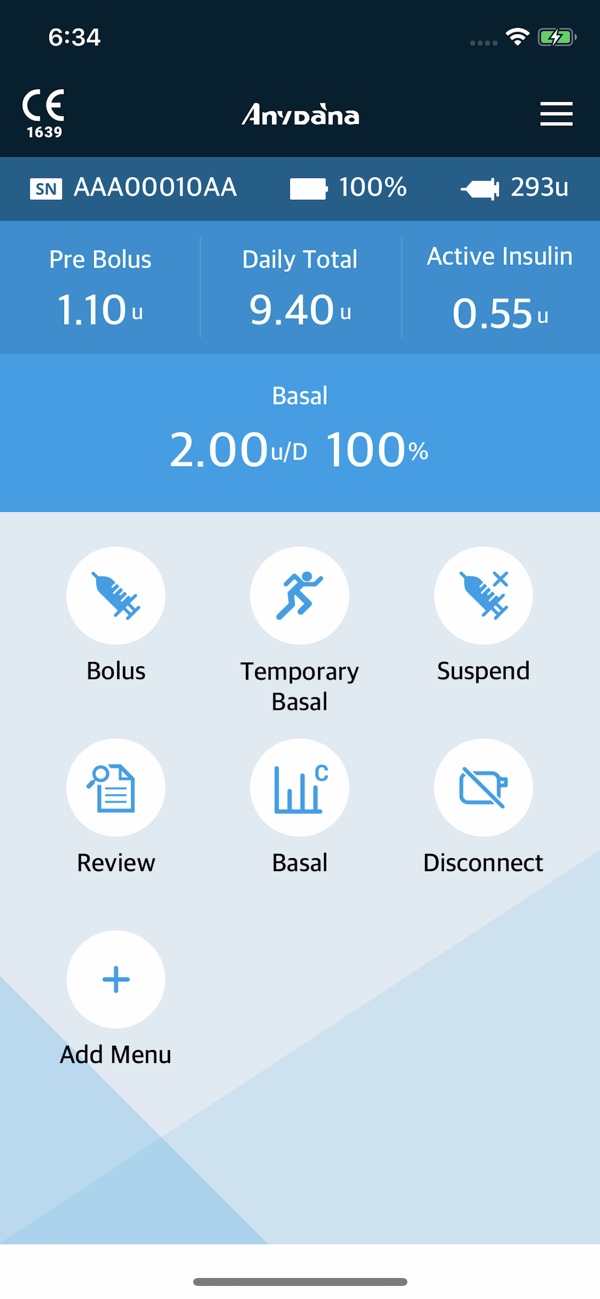
Immediately after being diagnosed with diabetes, I wondered if I could use an insulin pump myself, but unfortunately, there is not one on the market yet that includes a voice output. Fortunately, I managed to find a device that allows for connection with a smartphone, which I saw as a solution. And as you can probably guess, quite successfully. The insulin pump that can be connected to the phone is called Dana Diabecare RS and is distributed in the Czech Republic by MTE. I contacted this company about three weeks after leaving the hospital to ask if I could use the pump as a visually impaired person. Company representatives told me that neither MTE nor any other company in the Czech Republic has yet delivered a pump to a visually impaired customer, however, if everything goes well, we could come to an agreement.

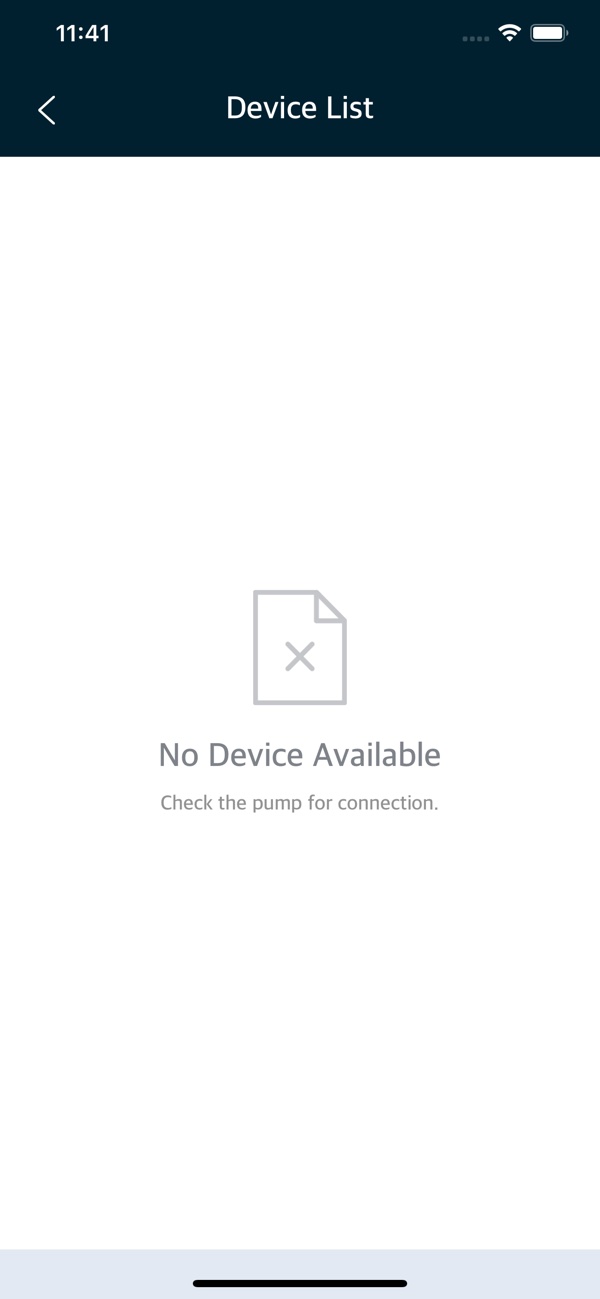
The cooperation at MTE was top-notch, I was able to test both the Android and iOS applications. Accessibility for the visually impaired was not the best, but after cooperation with the developers, it has moved forward significantly. The result was that I was the first blind patient in the Czech Republic to receive an insulin pump after three months. I use the AnyDana application for operation, which is available for both the Android and iOS operating systems.
You can try the AnyDana application here
But an accessible application is not everything
In the current situation, I perform both insulin administration and various advanced settings on the iPhone. I see a huge benefit in being discreet, where no one can see if I'm scrolling through Instagram, replying to someone on Messenger, or injecting insulin. The only action that is quite complicated to handle blindly is drawing insulin into the reservoir. Before piercing the cannula, I always have to change the reservoir with the insulin, which I have to draw from the bottle. On the one hand, as a blind person, I don't know if the bottle is already empty, in addition, I need to be able to recognize how much insulin I got in the reservoir when I draw it from the lines. I will admit that I need the assistance of a sighted person to do this, but fortunately, others in my family and in the group of friends in which I move around will help me with this. In addition, the reservoirs can be pre-filled and pre-prepared, thanks to which I can, for example, travel prepared to events where no one would be able to help me with the task.
It could be interest you

Blindness and diabetes, or it goes together
I have been suffering from diabetes for more than a year and a half, and in my case, I would rather describe diabetes as such an annoying cold. Primarily thanks to family and friends, great cooperation with the MTE company, and also modern technologies. If I don't count the current covid situation, I can now devote myself fully to all the activities I have been involved in so far. Apart from studies, these include writing, sports and playing musical instruments.